In 1988, Reaven described
metabolic syndrome (MS) as a set of clinical and laboratory alterations associated with an increased risk of cardiovascular disease. Although there is still no consensus regarding the components of the syndrome, it is known that hyperinsulinemia and insulin resistance (IR) are frequently present and are central factors in the development of complications. The most relevant aspect in the diagnosis of MS is represented by the risk of early development of type 2 diabetes
mellitus (DM2) and atherosclerotic cardiovascular disease (CVD). Regarding mortality, individuals with MS have higher rates of total mortality from CVD when compared to those without the syndrome. The
following are considered risk factors for MS: overweight/obesity, especially if there is accumulation of predominantly abdominal fat; dyslipidemia; systemic arterial hypertension (SAH) or CVD; personal history of glucose intolerance or gestational diabetes; family history of DM2, SAH or CVD; presence of
acanthosis nigricans and polycystic ovary syndrome (PCOS). Recent studies, however, suggest that MS may begin in fetal life, as can be observed in the monitoring of children born small for gestational age (SGA).
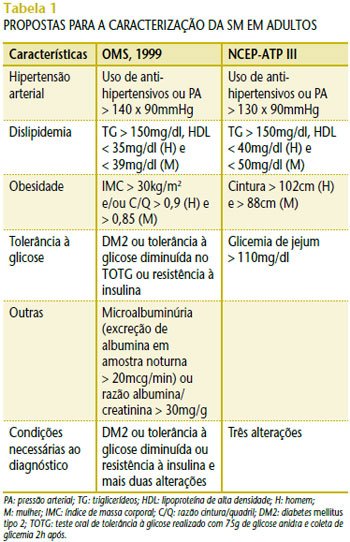
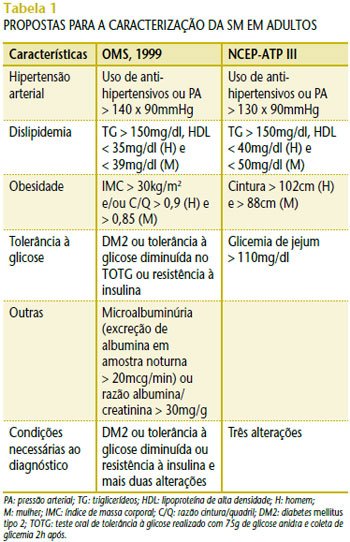
Most studies consider the guidelines of the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) and the World Health Organization (WHO) as parameters for the characterization of MS in adults. For the diagnosis of MS, the individual must present at least three of the alterations demonstrated in Table 1. The WHO considers the alteration in glucose metabolism a necessary condition for the diagnosis.
The main objective of establishing arbitrary criteria for the diagnosis of MS is to identify individuals at very high risk of complications and to use this information to initiate lifestyle changes that improve the prognosis of these individuals.
However, the epidemic of DM2 in childhood and adolescence in recent years, with the consequent early onset of serious complications, has raised the need to develop criteria for identifying risk early, even in childhood and adolescence. In the United States, in a sample of adolescents included in the III National Health and Nutrition Examination Survey (NHANES III), conducted between 1988 and 1994, the prevalence of MS was 6.8% among overweight adolescents and 28.7% among obese adolescents. These data may underestimate the extent of the problem due to the magnitude with which obesity has increased in prevalence in the last decade. More recent studies show that the prevalence of MS increases with the severity of obesity and can reach 50% in adolescents with severe obesity. Furthermore, the prevalence of MS is directly related to the decrease in insulin sensitivity that occurs in obesity, being a central factor in the genesis of complications.
Recent data released by the Brazilian Institute of Geography and Statistics (IBGE) based on the Household Budget Survey (POF) conducted in 2002-2003 shows that, of the 35.5 million adolescents aged 10 to 19, 16.75% are overweight and 7.3% are underweight for their age. For males, there was a 50% increase in the prevalence of overweight compared to 1989. Malnutrition is still a problem in Brazil, although a reduction has been observed in all regions and social classes, but obesity is emerging as a new challenge for society and the government. The probability of an obese child becoming an obese adult increases with age and the severity of the obesity, while a reduction of just 5% to 10% in weight significantly reduces the risk of future complications.
ROLE OF INSULIN RESISTANCE IN METABOLIC SYNDROME
IR is considered an isolated cardiovascular risk factor, since insulin, in addition to its role in glucose uptake, has other vascular effects, and IR is a frequent finding in hypertensive patients. There is also a strong association between central obesity and hyperinsulinemia. Although IR can occur in the absence of obesity, the prevalence of hyperinsulinemia and IR increases proportionally to the body mass index (BMI), especially when there is accumulation of abdominal fat, which is directly related to the accumulation of visceral fat. Visceral adipose tissue has as its main components non-esterified fatty acids (NEFA), which, in addition to being the body’s main caloric reserve, are considered important mediators of the effects of adipose tissue as an endocrine organ through the production of adipocytokines, involved in the pathophysiology of MS.
The relationship between IR and menstrual irregularity due to chronic anovulation (polycystic ovary syndrome [PCOS]) has been described by many researchers. The similarity in molecular structure between insulin and
insulin-like growth factor (IGF) allows a cross-reaction between the two, stimulating ovarian thecal cells and increasing androgen production, which results in inappropriate extraglandular conversion of estrogens. Consequently, there is an increase in the secretion of gonadotropins, particularly luteinizing hormone (LH), which also stimulates thecal cells to produce androgens. The effects of IR are potentiated in obese patients with PCOS, and it is also a common finding in non-obese patients with PCOS, who have a higher prevalence of dyslipidemia and an increased risk of developing DM2 and CVD characteristic of MS. This issue should be considered, since many adolescents who seek health services due to menstrual irregularities may have previously undiagnosed comorbidities such as arterial hypertension and dyslipidemia.
METHODS FOR DIAGNOSING METABOLIC SYNDROME IN CHILDREN AND ADOLESCENTS
As with adults, the presence of three or more risk factors is required for the diagnosis of MS.
1. Dyslipidemia: the characteristic lipid profile of MS is increased triglycerides and reduced high-density lipoprotein cholesterol (HDL-C). The proposed reference values for children and adolescents according to the recommendations of the I Guideline for the Prevention of Atherosclerosis in Childhood and Adolescence are shown in Table 2(1).
2. Arterial hypertension: SAH is defined as systolic blood pressure (SBP) and/or diastolic blood pressure (DBP) being greater than or equal to the 95th percentile for sex, age and height percentile on three separate occasions. In Brazil, we do not have a reference table for our population; we use the American table(2).
3. Obesity: BMI is defined as weight in kilograms divided by height in meters squared. Children whose BMI is between the 85th and 95th percentiles are considered overweight, and obese if BMI > 95th percentile, according to the reference charts prepared by the National Center for Health Statistics (NCHS).
4. Glucose tolerance: fasting blood glucose alone is not sufficient, in most cases, to demonstrate changes in glucose metabolism, and IR must be demonstrated. Several methods are described in the literature to assess IR, with the gold standard for this assessment being the euglycemic-hyperinsulinemic
clamp , which is not feasible to perform in clinical practice. Several simpler methods have already been standardized in relation to the
clamp . The
homeostasis model assessment insulin resistance (HOMA-IR) is the most sensitive and specific method for assessing insulin sensitivity, and is calculated using the following formula: glucose (mMol/l) x insulin (mMol/l)/22.5. The cutoff point for adolescents is 3.16, different from that for adults.
The American Diabetes Association (ADA) recommends the oral glucose tolerance test (OGTT) with 75g of anhydrous glucose and fasting glucose measurement and after 2 hours, for children over 10 years of age with a family history of DM2 in first or second degree relatives and conditions associated with IR such as
acanthosis nigricans , PCOS, SAH or dyslipidemia.
The interpretation of the OGTT is the same as for the adult population, that is:
Fasting glucose >126mg% = diabetes
mellitus .
Blood glucose 2h after anhydrous glucose:
- 140-200mg%: glucose intolerance;
- >200mg%: diabetes mellitus .
TREATMENT OF METABOLIC SYNDROME
Although there is no consensus on the criteria for identifying MS in children and adolescents, early intervention is important for all risk factors, whether they are present alone or in combination, according to the definition of the syndrome. Treatment of MS should be based on lifestyle changes, dietary reeducation, and encouragement of physical exercise.
The goals of treatment are weight loss, blood pressure and lipid control, which can be achieved through a diet appropriate for the age group, with restriction of sugars, saturated fats, and increased fiber intake. The use of medications is indicated for patients diagnosed with DM2, with metformin being the only medication approved by the Food and Drug Administration (FDA) for children and adolescents.