Abstract:
The increase in the incidence of eating disorders in adolescence and also in children increases the responsibility of the pediatrician in recognizing them. Early diagnosis is of fundamental importance, since it undoubtedly changes the long-term prognosis. The identification of other pathologies in the differential diagnosis is necessary. The approach is multidisciplinary and pediatricians are recommended to get involved in the treatment in different situations and at different critical moments of the disease. This article reviews the main clinical and therapeutic aspects of anorexia nervosa and bulimia.
Adolescence; eating disorders; diagnosis; treatment
Abstract:
The increase in eating disorders in adolescence and also in children increases the responsibility of the pediatrician in recognizing it. It is important to diagnose it in the beginning, because it changes the prognosis in a long run. The identification of other diseases in a differential diagnosis is totally necessary. The boarding is mustidiscipline and recommends to the pediatricians to involve their selves in the treatment in differents situations as well as in differents critical moments of the disease. This article makes a review of the main clinical and therapeutical aspects of eating disorders.
SUBTYPES
- Refusal to maintain weight within limits considered normal for height and age (below 15% of the weight considered ideal);
- fear of gaining weight;
- severe body image disturbance, measured predominantly by self-assessment, with denial of the severity of the illness;
- absence of menstrual cycles or amenorrhea (more than three cycles)
In reality, patients with anorexia nervosa do not have a loss of appetite, but rather a voluntary control over food intake. BULIMIA NERVOSA
- Restrictive: restriction of intake and intense physical exercise to induce weight loss;
- binge eating/purging: compulsive eating and purging (self-induced vomiting, laxatives, diuretics, and/or enemas) as a means of weight control.
Despite these behaviors, bulimic patients, in most cases, present with normal weight or with slight overweight. PHYSICAL EXAMINATION Weight, height and body mass index (BMI = kg/m2) should be measured regularly and can be useful in the diagnostic suspicion(1). FREQUENT PHYSICAL SIGNS(1,3,6,11) ANOREXIA NERVOSA
- Episodes of excessive eating with a feeling of loss of control;
- excessive intake compensated by self-induced vomiting; abuse of purgatives; alternating periods of starvation; use of drugs such as anorectics, thyroid preparations or diuretics;
- excessive eating and compensatory behaviors at least twice a week (for three months);
- dissatisfaction with body shape and weight.
BULIMIA
- Hypercarotenemia;
- xeroderma;
- alopecia;
- lanugo;
- bradycardia (heart rate [HR] < 60 bpm);
- hypotension (systolic blood pressure [SBP]<90);
- orthostatic hypotension;
- hyperactivity;
- difficulty concentrating;
- cyanosis of the nail bed.
DIFFERENTIAL DIAGNOSIS(6)
- Enlargement of salivary glands;
- erosion of tooth enamel;
- cheilitis;
- gingivitis;
- lesions and calluses in the proximal interphalangeal joints (Russel’s sign);
- the physical examination may be completely normal.
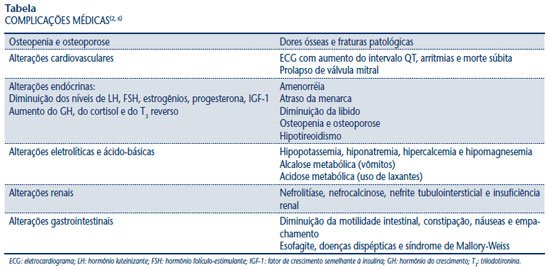
Adolescents with type 1 diabetes mellitus (DM1) are more likely to develop anorexia nervosa, and a common strategy for weight loss is to stop taking insulin(12). TREATMENT Treatment requires a multidisciplinary team consisting of a psychiatrist, psychologists, pediatrician (or general practitioner) and nutritionist(5). NON-PHARMACOLOGICAL TREATMENT(4-6) Nutritional therapy should be initiated with a supply of 1,000 to 1,600 calories/day or 30 kcal/kg/day, with gradual increases. The recommended weight gain is 200 g to 500 g per week and a maximum of 1 kg per week for hospitalized patients. In the initial phase of dietary treatment, severe hypophosphatemia and/or hypokalemia may occur in extremely malnourished patients due to the passage of phosphorus and potassium from the extracellular to the intracellular environment along with glucose. This is called refeeding syndrome, caused by the action of insulin, which can lead to cardiac arrhythmias and even death(4-6). Changes in eating behavior should be achieved through individual psychotherapy, cognitive-behavioral therapy and family therapy(6). PHARMACOLOGICAL TREATMENT ANTIDEPRESSANTS Serotonin reuptake inhibitors (fluoxetine hydrochloride): the results in anorexia nervosa have been disappointing, although they seem to benefit patients with comorbidities such as depression and obsessive-compulsive disorders, in addition to reducing relapses. In bulimia, the clinical response seems to be more effective, especially at a dose of 60 mg/day(4-6,9,10). Other antidepressants may be used, such as tricyclics, monoamine oxidase (enzyme) inhibitors (MAOIs) and buspirone. However, due to their side effects, fluoxetine is recommended as the first therapeutic option(4,5,9,10). ANTIPSYCHOTICS These may be considered in resistant, agitated patients with severe body image distortion. Olanzapine (2.5 to 10 mg/day) or risperidone (0.5 to 2 mg/day) are recommended(4,5,9,10). HORMONE REPLACEMENT WITH ESTROGENS The objective would be to minimize the impact on changes in bone metabolism, but its use remains controversial. Some studies have recommended the use of insulin-like growth factor (IGF-1) and dehydroepiandrosterone (DHEA), as they would favor the recovery of bone mass. It is recommended to ingest 1,200 to 1,500 mg of calcium per day and 400 IU of vitamin D(6,8,13,14).
- Diabetes mellitus (DM);
- adrenal insufficiency;
- primary depression with anorexia;
- diseases of the gastrointestinal tract, inflammatory diseases;
- abdominal tumors;
- nervous system injuries that cause vomiting, appetite suppression and behavioral changes;
- chronic infectious diseases.
DISCUSSION Anorexia nervosa and bulimia are behavioral disorders that challenge physicians in their daily practice, and this challenge ranges from diagnosis to treatment. Most of the time, it is up to the physician to suspect the condition, without having the laboratory or pathognomonic imaging resources available. Despite the proposed diagnostic criteria (DMS-IV), most patients do not meet these criteria, which makes it difficult to recognize them. The diagnostic process requires astuteness, since it is essential to differentiate the condition from clinical pathologies that also present with weight loss, depressed mood, vomiting, among others. Regarding treatment, despite the available resources, the results are disappointing, with high relapse rates and little acceptance of the diagnosis by the patient and their family, especially in the early stages of the disease(4,5). Patients who arrive at the hospital with severe malnutrition and prolonged progression do not respond well to serotonin reuptake inhibitors, because they lack the substrate (tryptophan) necessary for the drug to act(3). At this stage, all efforts are directed toward adequate improvement of nutritional status and toward preventing death by starvation. Thus, eating disorders should be recognized as serious clinical conditions associated with high rates of morbidity and mortality. Greater efforts are needed to modify current issues related to weight, especially with regard to the false idea of individual success with thinness.
- Severe forms of the disease (weight less than 75% of ideal);
- complications of malnutrition (seizure, heart failure, arrhythmia, etc.);
- unfavorable outpatient evolution;
- uncontrollable vomiting;
- psychiatric emergency (suicidal ideation).
Rua da Conceição, 100, Centro, Niterói, RJ, Postal Code: 24020-085, Brazil.
revista@adolescenciaesaude.com