INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of death worldwide. In Brazil, CVD accounts for 32.3% of deaths(1), accounting for approximately 250,000 deaths per year in the country(2). CVD is also the main cause of early mortality and morbidity. A comprehensive and truly effective prevention strategy requires a better understanding of the risk factors (RFs) for the development of this disease, which will allow for the development of better planning to direct public health policies with the aim of reducing the negative impact of CVD on the population.
The literature indicates that exposure to various cardiovascular RFs begins in childhood and adolescence. In younger individuals, modifiable RFs are crucially important because they tend to recur and worsen over the years. These data reinforce the need to initiate primary prevention early in these populations(3).
Even with advances in CVD therapy, mortality and related morbidity rates remain high. It is therefore evident that prevention is still the best strategy for addressing CVD and that knowledge about blood pressure (BP) and other RFs in young Brazilian populations is of great importance for the adoption of primary prevention measures in the country(4).
The present study aims to evaluate BP, anthropometric profile (weight, height, and body mass index [BMI]), and metabolic variables in young individuals from the Rio de Janeiro Study cohort and stratified by their BP behavior (tracking
) obtained on three occasions during 16 years of follow-up, from childhood and adolescence.
METHODOLOGY
The population of this study originated from the Rio de Janeiro Study, a line of research on BP and other cardiovascular RFs in young individuals and their families that has been developed at the State University of Rio de Janeiro (UERJ) since 1983. This study was conducted in two stages. In the first phase, 3,109 children aged 6 to 9 years (1983-1986) were evaluated in two phases: school and home. In the second phase, 3,906 children and adolescents aged 10 to 15 years (1987-2000) were evaluated in four phases: school (1987-1988), home (1989-1991), hospital (1992-1995) and family (1996-1999). Continuing this line of research, the fifth phase of evaluation began in 2004 (2004-2006), called the outpatient phase, which includes the present study (
Figure )(5-10).
Figure – Rio de Janeiro Study Design: second stage
Sixty-one young individuals (target students) of both sexes, selected for outpatient investigation, were evaluated. Three evaluations (A1, A2, and A3) were considered in the second stage of the Rio de Janeiro Study, namely: A1 (school phase – 10-15 years, 1987-1988); A2 (family phase – 18-25 years, 1996-1999), and A3 (outpatient phase – 26-31 years, 2004-2005). In the three evaluations, BP, weight, and height were obtained, and BMI was calculated. In A2 and A3, glucose, cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides (TGs) were also measured after a 12-hour fast. In A3, abdominal circumference (AC) measurements were added.
According to BP
tracking , three groups were formed: group N (normal BP in the three assessments; n = 27; mean age: 29.1 years); group L (variable BP in two assessments, with migration between BP values;
n = 26; mean age: 29.9 years); and group H (abnormal BP in the three assessments;
n = 8; mean age: 30.1 years).
Once contacted, the individuals were referred to the outpatient clinic of the Hypertension Sector of the Cardiology Service of the Pedro Ernesto University Hospital (HUPE) and, after signing an informed consent form, were evaluated.
The monitoring of these individuals included the application of a questionnaire to analyze clinical, epidemiological, metabolic and sociocultural variables, clinical and anthropometric evaluation, and obtaining blood samples for analysis. The information collected was stored in a database using Microsoft Access.
CLINICAL AND LABORATORY VARIABLES
All individuals were examined in an outpatient setting. The questionnaire applied included identification and socioeconomic data, clinical complaints, comorbidities and lifestyle habits. The physical examination included measurement of BP, heart rate and anthropometric variables.
BLOOD PRESSURE MEASUREMENT AT REST
BP was measured in the right upper limb, with the individual lying down, using a mercury column sphygmomanometer, fixed to the wall, with the zero point located at the level of the midaxillary line. Cuffs of size and width appropriate for the circumference and length of the individuals’ arms were selected, according to the standards of the American Heart Association (AHA). The appearance of the first Korotkoff sounds (Korotkoff phase I) was considered for SBP, and the disappearance of the sounds (Korotkoff phase V) for DBP. Three BP recordings were made, with 5-minute intervals between each measurement, with the last one being used for analysis. Arterial hypertension (AH) was considered in A1 when BP
>95th percentile for sex and age and in A2 and A3, BP
> 140/90 mmHg.
ANTHROPOMETRIC ANALYSIS
The assessment of body composition was performed in fasting conditions, and the following anthropometric variables were considered for this study, through records and a single examiner:
a) weight (W) – the measurement was taken on a Filizola platform-type scale with a capacity of up to 150 kg, accuracy of 100 g, and values expressed in kilograms (kg);
b) height (H) – the measurement, with its values expressed in centimeters (cm), was taken on the same scale, considering the distance from the vertex point to the plantar region, with the individuals standing erect and without shoes;
c) BMI – the BMI was calculated from the weight and height measurements, expressed in kg/m2
, using the quotient BMI = W/H2. BMI values < 25 kg/m² were considered normal weight; overweight, BMI values between 25 kg/m² and 29.99 kg/m2; and obesity, BMI values
> 30 kg/m2
, according to the World Health Organization (WHO)(11).
WAIST MEASUREMENT
Waist measurement (WC) was obtained using a non-stretchable tape measure, with an accuracy of 0.1 cm, measured in centimeters, with the subject in the orthostatic position, parallel to the ground and with the abdomen relaxed. The measurement was taken horizontally, with the tape firmly on the skin and without pressure on the tissues, at the midpoint between the iliac crest and the lower edge of the last rib, according to the procedure described by Callaway et al. in 1991(12). Increased values were defined as WC
> 94 cm for men and
> 80 cm for women, according to the WHO standard in 1997(11).
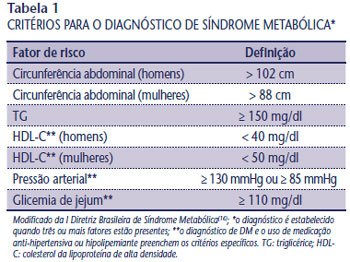
METABOLIC SYNDROME
The presence of metabolic syndrome (MS) was defined according to the I Brazilian MS Guideline(13) (
Table 1 ).
LABORATORY ANALYSIS
Venous blood samples were collected in the morning, up to 8:30 a.m., by puncture of a peripheral (ulnar) vein in the arm, under standard conditions and after a fasting period of 12 hours or more. All samples were stored in siliconized vacuum tubes, and aliquots for glucose measurement were kept in tubes containing sodium fluoride. The samples were processed within a maximum period of 30 minutes, and the measurements were performed on serum obtained after centrifugation at a speed of 3,500 revolutions per minute for 5 minutes. Part of the serum was stored in a
freezer at -80° Celsius in order to keep it viable for a long time for future analyses.
The data were analyzed using the statistical program SPSS for Windows, version 8.0.0, Copyright SPSS Inc. 1989-1997.
RESULTS
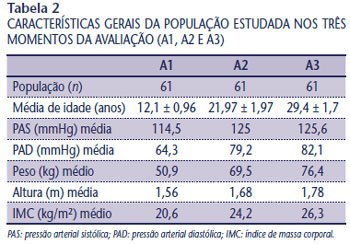
To date, 61 individuals have been evaluated, 47.6% male (29) and 52.4% female (32). The results did not differ in terms of age or sex. Table
2 shows the general characteristics of the study population at the three evaluation times (A1, A2 and A3); the mean follow-up was 199.38 ± 4.56 months.
Three groups were formed according to the study characteristics (BP assessment): group N (normal BP in the three assessments) with 27 individuals (17 F/10 M), group H (abnormal BP in the three assessments) with eight individuals (4 F/4 M) and group L (variable BP in the three assessments) with 26 individuals (10 F/6 M).
Groups H and L showed higher SBP and DBP means than group N in A1, A2 and A3 (
p < 0.001), as shown in
Table 3 .
The prevalence of hypertension, defined at A1 as BP
> 95th percentile for sex and age and at A2 and A3 as BP
> 140/90 mmHg, was 44.3% (27/61); 24.6% (15/61) and 32.8% (20/61) at A1, A2 and A3, respectively.
Group H showed higher mean weight and BMI than group N at A1, A2 and A3 (
p < 0.003) (
Table 4 ). At A3, the prevalence of overweight in groups N, H and L were 30.8%, 100% and 76.9%, respectively (
p < 0.001). In the group of 61 individuals studied, 60% were overweight or obese at A3.
There were no differences regarding metabolic variables in A3 (
Table 5 ).
MS was detected in 40% of the individuals in group H and was not found in any individual in group N (
p < 0.03) in A3.
DISCUSSION
Understanding the behavior of cardiovascular risk factors over the years is of fundamental importance, since they favor the development of changes in the cardiovascular system. Several epidemiological studies have been developed over the last decades with the objective of understanding the cardiovascular risk profile in children, adolescents and young adults(5-10, 14).
BP tracking
has been analyzed in several populations of young people(5, 6, 8-10, 14). In one study, 481 schoolchildren were evaluated from 6 years of age for a period of nine years. Among the children with SBP means located in the highest quartile in the first evaluation, 70% remained in that same quartile after nine years; in contrast, more than 90% of the children who were not in the highest quartile in the first evaluation remained outside it after nine years(15). Suh et al. recruited 219 children older than 6 years in Kangwha for annual assessment between 1986 and 1997. These authors found a correlation coefficient for SBP
tracking between 6 and 17 years of age of 0.39-0.54 for males and 0.44-0.57 for females, and for DBP, of 0.28-0.47 in males and 0.14-0.47 in females. These findings demonstrate the presence of BP
tracking in Korean children up to adolescence(16). In the present study, the mean SBP and DBP in the three assessments showed statistically significant differences, which was expected, since BP was the stratifying factor of the study population. In the two-by-two comparison, the mean SBP and DBP in group H were higher than those observed in groups L and N over the 16 years of follow-up (A1: SBP and DBP – H = L > N [
p = 0.001]; A2: SBP and DBP – H > L = N [
p = 0.001]; A3: SBP – H > L [
p = 0.009] and H > N [
p = 0.001] and DBP – H > L [
p = 0.002] and H > N [
p = 0.001]). Weight is a very important variable when studying cardiovascular risk in young populations. The first results of the classic Bogalusa Study demonstrated that the descendants of patients with early coronary artery disease (CAD) were overweight from childhood and developed, throughout adolescence and young adulthood, an extremely unfavorable cardiovascular risk profile(14).
In 2001, Burke et al. published a study of Australian children. They found an increase from 34%-48% to 60% in BP tracking among children with BMI in the highest quartile and to 70% in those whose BMI varied throughout the follow-up. The results suggested that excess weight in adolescence and a family history of hypertension increased the risk of hypertension maintained in adulthood(17).
In the Rio de Janeiro Study, individuals in group H had higher weight and higher BMI when compared with individuals in group N (
p < 0.003). A positive association was also found between overweight and hypertension in phase A3 of the study, demonstrated by the prevalence of overweight/obesity of 100%, 76.9% and 30.8% in groups H, L and N, respectively (
p < 0.001). In this phase (A3), the prevalence of systemic arterial hypertension (SAH) was 32.8%, and that of overweight/obesity was 60%.
The Amsterdam Growth and Health Study, which investigated RFs related to lifestyle (diet, physical activity, smoking and alcohol consumption) and also the so-called biological ones (lipoproteins, BP, anthropometry and physical fitness), demonstrated that the repetition coefficient for lipoproteins was able to predict the metabolic profile of young adults(20).
The results of the Bogalusa study demonstrated the presence of tracking for lipid and lipoprotein values from childhood to adulthood. Similarly, abnormal low-density lipoprotein (LDL) values in childhood persist over time, progressing to dyslipidemia in adulthood; these findings are usually associated with obesity and hypertension. The autopsy findings and noninvasive examinations performed by researchers in Bogalusa’s group were able to demonstrate the association between the aggregation of multiple RFs and changes in the cardiovascular system. Individuals with none, one, two, three or four RFs had 19.1%; 30.3%; 37.9% and 35% of the endothelial surface of the aorta covered by fatty streaks (
p = 0.01)(18).
In this evaluation (A3) of the Rio de Janeiro Study population, no statistically significant differences were observed between the lipid variables studied; however, these variables were not studied longitudinally in these individuals.
Clinical studies have contributed to expanding the knowledge that MS, with all its constellation of complex associations with traditional RFs, emerges as one of the main challenges in medical practice, since it is known that the presence of MS multiplies cardiovascular mortality, increasing the risk by 2.5 times(13).
In the Aerobics Center Longitudinal Study(19), 48 individuals were evaluated at two time points: in adolescence (mean age of 15.8 years) and in adulthood (mean age of 26.6 years). The results obtained demonstrated that MS had a repetition coefficient of 0.56 from adolescence to adulthood.
In the Rio de Janeiro Study, MS was present in 40% of the individuals in group H and was not observed in group N (
p < 0.03) in A3.
CONCLUSION
It is recognized and indisputable that RFs are involved in CVD in adults and the elderly; however, information on their implications in children, adolescents and young adults is still limited(18).
In this context, the findings of the Rio de Janeiro Study, in 16 years of follow-up, demonstrated a significant correlation between the BP behavior of young individuals from childhood to adolescence, anthropometric variables and the occurrence of MS. These findings represent a preliminary analysis within a longitudinal evaluation in which the loss of individuals from the study cohort over time has been the main limitation. Despite this, they reinforce the importance of early identification of traditional cardiovascular risk factors that can potentially allow the establishment of early prevention and intervention strategies for these conditions in this age group, with the aim of reducing the high rates of morbidity and mortality from CVD in adulthood.