INTRODUCTION
Social disparities in access to health services have gained prominence in public health research, aiming to acquire subsidies for new policies that support the provision of services in a universal and equitable manner.
1
When it comes to socially excluded populations, such as those living in rural and remote areas, the difficulties in access are evident given the scarcity of health units installed in rural areas, the lack of infrastructure in health promotion sites, and the lack of motivation of professionals to work in remote areas, aggravated by the lack of affinity and commitment to public service
1 .
Rural settlements originated in the search for agrarian reform. Unproductive lands are invaded by landless families, where they camp without any sanitary conditions. After the concession and division of the lands, the families go from being campers to settlers, forming a rural settlement
2 .
In Brazil, residents of rural settlements receive care from doctors, dentists and nurses who work in health centers in rural areas, as the government has guaranteed investments that support the implementation of these centers in order to prevent harmful habits, behaviors that are detrimental to health and chronic diseases
2 .
With regard to dental care, inequitable access among rural populations can culminate in the worsening of oral diseases, resulting in irreversible losses and damages and impairments in quality of life
3 . Among oral problems, caries and periodontitis stand out because they predominantly affect rural populations, generating social losses for individuals. Habits and lifestyle can interfere with oral health, increasing the chances of developing these diseases
4 .
The DMFT index (decayed, missing and filled teeth) is around three among Brazilian adolescents aged 11 to 14, and almost six among young people aged 15 to 19 and residents of rural areas
5 . When flossing is not a common practice, there is a greater likelihood of gingivitis and periodontitis occurring, compromising the fixation of teeth in the jaws
6 . The lack of care for populations with this dental condition tends to result in a population of edentulous young adults, and the corresponding losses and damage to general health
5 .
Given the disparities in access to oral health services, it is challenging to follow a non-cariogenic diet, brush and floss daily, and avoid harmful habits such as alcohol and tobacco consumption, to avoid acquiring oral diseases
6. In this regard, the objective of this research was to verify the behavior, habits and oral health status of Brazilian adolescents from rural settlements in view of the inequitable access to dental services.
METHODOLOGY
A cross-sectional epidemiological study was conducted with surveys, of an exploratory, descriptive and analytical nature, in which all adolescents from a rural settlement (Caiuá, São Paulo, Brazil) were invited to take part in the research. In the settlement there are two small villages with a Family Health Unit in each of them, offering medical, dental and nursing care. In one of these villages is the school that serves all rural adolescent residents of the municipality.
For the World Health Organization (WHO), adolescence comprises the age group between 10 and 19 years. Since in Brazil regular Elementary and High School includes young people between 6 and 17 years old, the research was conducted in the school itself, in which 349 adolescents are enrolled. Because they belong to low-income families, they receive financial assistance from the federal government (Bolsa Família) and, to maintain this assistance, the young people cannot miss school, thus facilitating the approach with the study population. Data collection was carried out during school hours, in a private location so as not to cause embarrassment and/or coercion. The research was approved by the Ethics Committee for Research with Human Beings of the Universidade Estadual Paulista – Faculdade de Odontologia de Araçatuba, and ethical rigor was followed in conducting the research.
Of all the adolescents interviewed and examined, only those whose parents/guardians authorized participation in the research, the young people who agreed, and those who allowed themselves to be examined by mouth were included in the sample. Students who were absent on the days scheduled for oral examination and/or interviews and who were not found after three consecutive subsequent attempts were excluded from the sample. The GSHS-WHO (
Global School-based Student Health Survey
) instrument, developed in 2003 by the WHO to assess health risk behaviors among adolescents, was used as the interview guide . The parts of the original instrument that addressed eating habits and BMI (Body Mass Index) (33 questions), oral hygiene habits and access to dental services (27 questions); alcohol consumption (24 questions) and tobacco consumption (6 questions) were explored
7 .
To assess the dental and periodontal condition of the adolescents, an oral examination was performed by a single calibrated researcher, whose intra-examiner Kappa test was 0.88, obtained in a pilot study previously conducted with other adolescents from other rural areas of the region, to adapt the methodology. The examinations followed the WHO guidelines for epidemiological studies.
During the oral examination, the DMFT index of caries was assessed, which measures the number of decayed, missing and filled teeth, and the CPI (Community Periodontal Index), which assesses the periodontal/gingival condition of the maxilla and mandible, according to sextants, classifying them as healthy (CPI=0), presence of gingival bleeding (CPI=1), dental calculus (CPI=2), periodontal pocket between 4 and 5 mm in depth (CPI=3) and periodontal pocket with 6 mm or more (CPI=4). A descriptive analysis of the data was performed to characterize the sample; then, bivariate analyses were performed, the Chi-square test or Fisher’s exact test was applied with a 95% confidence interval for both. The BioEstat 5.3 and SPSS 20.0
software were used . Multivariate logistic regression analysis was applied to the variables that were statistically significant in the bivariate analyses.
RESULTS
Among the 349 students who studied at the rural school, 15.2% moved from the settlement to other areas/cities during
the research period, 4.3% stopped studying, 0.6% died; 2.3% refused to participate in the research or did not have authorization from their parents/guardians, 26.4% did not answer all the interview questions or did not allow an oral examination. The final sample consisted of 179 adolescents.
Regarding access to dental services, 55.3% had consulted a dentist in the last 12 months, the remainder had consulted one two years ago or more, or had never consulted one. Among the 177 who had already visited a dentist, the main reason for the last consultation was pain resulting from some problem in the teeth/gums (69.5%), followed by routine consultations (16.4%) and continuity of dental treatment (14.1%).
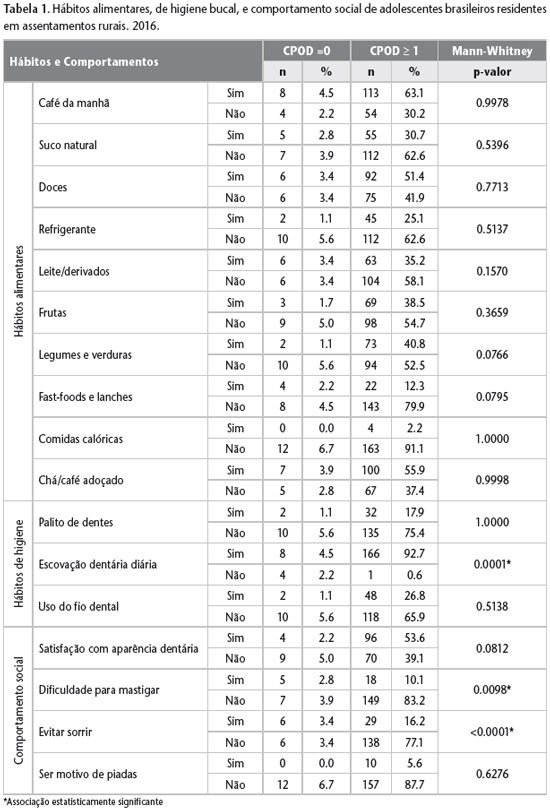
Data regarding eating and oral hygiene habits, social behavior in relation to one’s own oral health condition and the result of the Mann-Whitney test between the variables are presented in Table 1.
Habits regarding alcohol and tobacco consumption are presented in Table 2. There was no association between alcohol and tobacco consumption with dental caries or gingivitis/periodontitis. Among the interviewees, 13.4% were overweight.
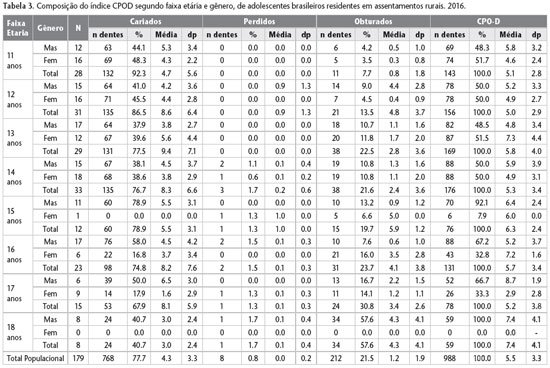
Table 3 shows the composition of the DMFT index by age, gender and index components. Among all treatment needs, restorative procedures were the most prevalent (97.3%). When asked about their self-perception of dental condition, 35.8% described it as “good”, 58.7% as “fair” and 5.5% as poor.
The IPC index ranged from 0 to 3 and 68.2% of the total did not present periodontal alterations. Analyzing the worst condition among all the sextants examined, it was observed that 24.6% of the interviewees had gingival bleeding (IPC=1), 6.7% had dental calculus (IPC=2) and 0.5% had periodontal pockets between 4 and 5 mm in depth (IPC=3). There was no sextant with deep periodontal pockets (≥ 6 mm in depth). The need for periodontal treatment focused on preventive actions with hygiene instructions (19.6%) followed by prophylaxis (2.7%). Regarding the self-perception of gingival health, 62.6% of the total described it as “good”, 33.0% as regular and 4.4% as poor.
In the bivariate analyses, when adjusting the data according to the median of the DMFT index (median = 5), an association was observed between a high prevalence of caries (DMFT ≥ 5) and the following variables: obesity (p = 0.0435), reason for pain at the last appointment (p = 0.0011) and frequency of daily tooth brushing less than three times (p = 0.0048).
Regarding the periodontal condition, gingival bleeding was associated with the intake of high-calorie foods (p = 0.046), tooth brushing only once a day (p = 0.0172) and dissatisfaction with oral health (p = 0.0082); while calculus was associated with the intake of sweets, candies, chewing gum, chocolates (p = 0.0386) and with the routine reason at the last appointment (p = 0.0500). In the logistic regression model, there was an association only between dental calculus and the reason for the last consultation as being routine (p=0.0158).
DISCUSSION
Considering that the study population is assisted by two Family Health Units in the rural settlement, and that even so, they presented worse oral health conditions than the national average, whose DMFT is 4.28
, it is suggested that there is some problem in accessing dental services, since a little more than half of the interviewees consulted the dentist frequently, and because pain was the main reason for the consultation. It was also highlighted that, during the development of the research, analyses were made of the fluoride levels present in the artesian wells that supplied water to the residents of the location, and no significant levels of the ion were found (below 0.15 mgF/L), which is, therefore, another reason that may have contributed to the oral health condition found in the adolescents studied.
There are two ways to interpret inequality of access: first, as a gradient inversely proportional to
per capita income and educational level; second, as a serious problem among marginalized parts of a given population, characterized by lack of resources, opportunity, vulnerability and which contrasts with the rest of the population
.. When inequality in access to health care persists, regardless of how it is interpreted, the tendency is to find a population with poor oral health conditions, pain, suffering and significant tooth loss
10 .
Inequity in access to health services persists in many countries, regardless of the profile of each system. Although managers try to contain it by implementing new public policies seeking to expand population coverage and access to financing for new projects, the lack of specific legislation on accessibility and the long time expected to implement new strategies become the main barriers
11 .
Given the disparity in access, it is a great challenge to maintain good habits and lifestyle in order to prevent the worsening of oral health conditions, especially dietary habits. Young people in general have shown the same eating behavior all over the world, even though they come from different cultures and countries, as they have already adopted the inclusion of soft drinks, fruit juice, coffee and milk with added sugar in their daily diet
12 .
However, even when they practice good oral hygiene, most adolescents suffer from tooth decay (97%), due to the cariogenic action of the sugar present in these foods and the delay in dental hygiene. Poor hygiene among young people living in rural areas has prevented significant progress in reducing this disease
6 . Adolescents who are instructed on the proper brushing technique tend to improve their oral hygiene and, consequently, their dental and periodontal condition
13 .
Inadequate dental hygiene results in the accumulation of biofilm and consequent gum inflammation; when left untreated, gingivitis progresses and affects the periodontium, that is, the structures that support the teeth in the alveolar bone
4 . The higher the educational level, the lower the probability of developing moderate and severe periodontitis
4 .
Beer consumption has also increased among young people living in rural areas. Family environments, whose habits include the deliberate consumption of alcoholic beverages, encourage the same habits in their children who live in these environments, adhering to it from the beginning of adolescence
14. When observing the data, it was noted that the families of the young people interviewed raise their children in an environment that is hostile to the consumption of alcoholic beverages, making them more vulnerable to addiction and chemical dependency. Although the sale of alcoholic beverages is prohibited for minors under 18 years of age in Brazil, their consumption by young people would not be prevented, since their own family members would not prevent such a habit. After all, just over 8% reported that being underage was not an impediment to purchasing these beverages.
The population in this study does not have leisure options and therefore considers the use of alcoholic beverages as a form of entertainment, a habit that is common to almost all family members. On the other hand, the oral hygiene habits of consumers of alcoholic beverages are unsatisfactory and therefore result in halitosis and gum changes
15 .
Smoking also begins, which is also a contributing factor to the worsening of periodontitis and social damage; frequent smoking can increase by almost three times the chances of an individual developing periodontal problems
15 .
Overweight is another significant indicator of chronic diseases in adolescence, especially with regard to periodontitis
16 . The association between overweight and dental caries is due to the intake of a cariogenic diet, rich in sugar and carbohydrates. Obesity should be carefully considered in preventive programs, including the intention to avoid dental caries, especially with regard to interproximal lesions, and should include several health professionals such as dentists and nutritionists in the team.
17
The worsening of dental caries generates high rates of tooth loss among young adults, and consequently, “exodontia” is the most common procedure in dental treatment
2 . In developed countries, visits to the dentist are regular and preventive, since this is a multifactorial disease, which depends on the presence of specific bacteria, food debris, genetic predisposition, salivary pH, among other factors, which results in a low percentage of restorative and surgical procedures
6 .
Decayed teeth, pain and dental trauma are conditions that harm the quality of life of young people, but can be triggering factors for seeking dental treatment among them, since in social life, good appearance is a criterion for inclusion in some groups of friends
18 .
The data on the social behavior of young people in relation to oral health transcribe the social harm that the lack of oral care brings to the individual, culminating in suffering and tooth loss due to lack of care. It is worth noting that almost 20% of the population studied reported avoiding smiling in public because of the appearance of their teeth, and that almost half of the young people reported satisfaction with the appearance of their own teeth.
At this point, the intervention of professionals using health education to guide the community on the importance of oral hygiene and the risks resulting from lack of health care is justified. Consequently, this behavior could be considered a habit of the population in question and/or a lack of guidance on oral health. These studies with rural young people in a school environment are of utmost importance for maintaining the health of this population, as they achieve improvements in oral hygiene habits
1 and changes in eating habits
19 , especially when using methodologies with demonstration and participation of adolescents
20 .
In this study of oral health among adolescents living in a rural settlement, it was noted that inequity in access, habits, and behaviors can influence oral health status. It was concluded that difficulty in accessing dental services culminates in the worsening of caries and periodontal disease, impairing chewing and the social life of adolescents. Oral health status depends on the lifestyle, habits, customs, and behavior of young people, among other aspects. Obesity and low-frequency toothbrushing increase the risk of caries. The consumption of high-calorie foods and insufficient brushing result in bleeding gums. The persistent inequity in access to dental services by socially excluded populations needs to be combated through public health policies that achieve the principles of equity and universality, given the irreversible losses and damage to health, especially with regard to adolescents.