Objective: To determine the efficacy, safety, and usefulness of uniportal video-assisted thoracoscopic surgery (VATS) for decortication of empyema in paediatric patients. Study design: Case series Place & Duration of Study: Department of Cardiothoracic Surgery, Shifa International Hospital Islamabad, from September 2023 to May 2024. Patients and Methods: This study was carried out on patients who were admitted with post-pneumonic pleural effusion, for whom decortication of empyema was suggested, and uniportal video-assisted thoracoscopic surgery was performed. Results: A total of 7 patients with empyema thoracis underwent Uni-VATS. In all patients of empyema thoracis who underwent thoracoscopic decortication, surgery was performed successfully, and none of them converted to open thoracotomy. MRSA was the most predominant organism found in the blood culture of our patients. The postoperative hospital stay was relatively brief averaging around 5 days, and placement of chest drains was for a shorter period with minimal output. The long-term outcome was excellent with all the patients healthy without any recurrence. Conclusions: Uniportal VATS is a safe, effective, and minimally invasive diagnostic and therapeutic procedure in children. It has a low rate of complications and is particularly useful for thoracoscopic decortication, which is the optimal procedure of choice for empyema thoracic. As the learning curve progresses, more and more procedures are being adopted via minimally invasive uniportal VATS, and it is becoming an increasingly popular option for paediatric patients with outstanding results.
Dr. Diego Gonzalez-Rivas, a Spanish thoracic surgeon, introduced the Uniportal VATS technique in 2010. Since then, it has become popular worldwide among thoracic surgeons as a safe and effective alternative to traditional open surgery and multiport VATS procedures. While VATS has replaced thoracotomy, it usually involves multiple incisions or ports, which can lead to increased postoperative pain. However, Uniportal video-assisted thoracic surgery (Uni-VATS) is a minimally invasive approach that involves accessing the heart and lungs through a single small incision [1].
Uniportal video-assisted thoracic surgery (VATS) offers several advantages over conventional VATS. It minimizes surgical trauma, resulting in decreased postoperative pain, faster recovery, and reduced reliance on postoperative narcotics. Additionally, it shortens hospital stays, enhances postoperative lung function, and lowers the levels of inflammatory cytokines circulating in the body after surgery. Moreover, uniportal VATS improves the cosmetic outcome, leading to higher patient satisfaction compared to traditional VATS. It can be used for increasingly complex thoracic procedures through a single small incision, avoiding the associated risks of conventional open chest surgery, such as thoracotomy [2,3].
During the Uni-VATS procedure, the surgeon creates a small incision, approximately 2.5 cm long, without cutting the ribs. This incision serves as a port for specialized surgical instruments and a thoracoscope, a long, thin rod with a fibre-optic video camera. The thoracoscope allows the surgeon to visualize the pleural cavity and lungs and perform the surgery without the need to open the chest wall. Through this single, small incision, the surgeon can perform various procedures, ranging from lobectomy, empyema decortication, and pericardial window to pleurodesis, blebectomy for pneumothorax, sympathectomy for hyperhidrosis, Lung volume reduction surgery (LVRS), mediastinal surgeries, and even complex procedures like sleeve resections, bronchoplasty, repair of eventration of the diaphragm, and valves (mitral), ASD, and AF (atrial fibrillation), achieving excellent outcomes [4,5]
Empyema is referred to as purulent fluid in the pleural cavity. In the majority of cases, pleural space infection following post-bacterial pneumonia is to blame. Based on its radiological characteristics, exudative, fibrinopurulent, and organizing phases have long been identified as the three stages of empyema’s natural progression. Empyema can present with pleurisy, excessive sweating, particularly during the night, fever, malaise, chills, and breathing difficulty. It is treated by draining the pus from the pleural space and treating the infection, typically with antibiotics. In the early stages of empyema, a healthcare provider would remove pus by thoracentesis. In some instances, more sophisticated techniques like uniportal video-assisted thoracic surgery (VATS) are utilized, which has proved to be the treatment of choice for this condition; therefore, this study aimed to explore the efficacy, safety, and usefulness of uniportal video-assisted thoracoscopic surgery (VATS) for decortication of empyema in paediatric patients.
This retrospective study was conducted at the Department of Cardiothoracic Surgery, Shifa International Hospital Islamabad, using an online database via Electronic Medical Records. The study spanned nine months, from September 2023 to May 2024. All patients underwent a thorough history and clinical examination, followed by relevant investigations such as CBC, Chem7, CRP, Immunoglobulin, Blood culture and sensitivity, D-Dimer, COVID-19, Liver function tests (LFTs), Hepatitis B and C. Radiological investigations, including plain X-ray chest and HRCT scan chest, were also performed. Patients with other co-existing diseases received treatment before undergoing UNI-VATS. The study included patients ranging in age from 6 months to 8 years who underwent Uniportal video-assisted thoracic surgery (Uni-VATS) for empyema decortication resulting from post-pneumonic pleural effusion. This intervention was considered either when the patients demonstrated minimal or no response to antibiotics or when chest tube placement proved ineffective (in specific cases). Patients over the age of 16, those who underwent multi-portal VATS, or those who underwent Uni-VATS for indications other than empyema decortication were excluded from this study.
All surgeries were performed under general anaesthesia, with the patients being intubated. The procedure was performed with both lungs of the patient being ascended as a double lumen tube (DLT) of pediatric size and a bronchial blocker were not available. A small incision (2.5 cm) was made in the fifth intercostal space at the anterior axillary line. A rigid \(30^\circ\), 5 mm optic thoracoscope was used for visualization, and various specialized instruments were used through the incision. The surgery involved repairing septal rupture, removing debris, adhesions, and loculations from the visceral and parietal cortex to the apex of the chest cavity, and removing inflammatory fluids to create a single pleural cavity without septations. Multiple washings with a warm physiological solution were performed to remove any remaining fluid or pus from the lung lining. Following the surgery, a single 20 Fr chest tube was inserted through the incision site to drain the pleural space, and the patient was extubated. The tube was removed once there was no air leakage and the amount of daily drainage was less than 1 mL/kg. Patients were discharged one day after the chest tube removal, provided that the follow-up chest X-ray showed no signs of pneumothorax (collapsed lung) or complications. All the data were entered and analyzed using SPSS version 27.
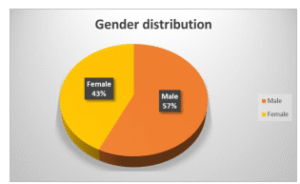
In our study, we examined a total of 7 patients who underwent Uniportal-VATS over 9 months. Out of these 7 patients, 4 (57%) were male, and 3 (43%) were female, resulting in a male-to-female ratio of 1.3:1. The mean age of the patients was 3 years and 6 months, ranging from 6 months to 18 years. The most common presenting complaints observed were fever and shortness of breath, which were present in almost all patients. Additionally, 2 (28.57%) patients also reported chest pain. On examination, diminished air entry was observed on the affected lung side in all patients. (see Figure 1).
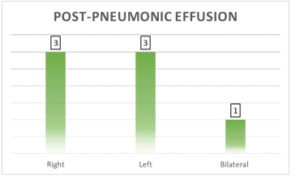
The most frequent diagnosis was post-pneumonic effusion, affecting the right lung in 3 (42.8%) cases, the left lung in 3 (42.8%) cases, and it was bilateral in 1 (14.3%) case. Among the patients, 2 (28.5%) had pneumothorax in addition to empyema, 1 (14.3%) had co-existing comorbidities of hepatitis A and emphysema, and 1 (14.3%) had septicemia. The blood culture results revealed MRSA in 4 (57.14%) patients, while one of them also had Bacillus along with MRSA, Streptococcus pneumoniae in 1 (14.3%) patient, pseudomonas in 1 (14.3%) patient, and no bacterial growth in the blood culture of 1 (14.3%) patient because he had empyema due to complicated COVID pneumonia. (see Figure 2).
The duration of hospital stay ranged from a minimum of 5 days to a maximum of 30 days, with an average stay of 14 days. Out of the patients, 5 (71.43%) had an average hospital stay of 5 days after the surgery, ranging from a minimum of 3 days to a maximum of 8 days. However, 2 (28.57%) of the patients had a hospital stay exceeding 15 days. Among these, one patient had a recurrence of lung collapse, while the other patient had an ongoing pneumococcal infection. Regarding the duration of post-operative drain placement, 3 (42.8%) patients had their drain removed after 1 day, and 3 (42.8%) patients had it removed after 5 days, resulting in an average of three days. However, one patient (14.3%) had the drain in place for 27 days due to recurrent lung collapse. No intra-operative complications were observed, and none of the surgeries required conversion to open thoracotomy or multiport VATS. Each patient had a single drain of 20 Fr placed.
The amount of drainage in the first 24 hours was 50 ml for 4 (57.4%) patients, while the remaining 3 (43.6%) patients had an average drainage of 156 ml. Air leak was reported in only 2 (28.57%) patients. Post-operative complications occurred in 1 (14.3%) patient who developed pneumothorax, pulmonary bleeding, and bradycardia, necessitating readjustment of the drain, suction, and CPR. (see Table 1).
| Parameters | N | % |
|---|---|---|
| Blood Culture Results | ||
| MRSA | 4 | 57.14 |
| Bacillus, along with MRSA | 1 | 14.3 |
| Streptococcus pneumoniae | 1 | 14.3 |
| Pseudomonas | 1 | 14.3 |
| No bacterial growth | 1 | 14.3 |
| Hospital Stay | ||
| Average of 5 days | 5 | 71.43 |
| \(>15\) days | 2 | 28.57 |
| Post-operative Drain Placement | ||
| Drain removed after 1 day | 3 | 42.8 |
| After 5 days | 3 | 42.8 |
| 27 days | 1 | 14.3 |
| Amount of Drainage in the First 24 Hours (ml) | ||
| 50 | 4 | 57.4 |
| 156 | 3 | 43.6 |
In terms of normalization of inflammatory markers, the process took a minimum of 3 days and a maximum of 25 days, with an average of 18 days. All patients exhibited a swift decline in inflammatory markers after the surgery, resulting in their discharge once their CRP levels significantly dropped. Subsequently, they were placed on oral antibiotics for follow-up until their inflammatory markers returned to normal levels.
In the field of cardiothoracic surgery, there has been remarkable progress and development over time. Initially, open thoracotomies were conducted to gain access to the thoracic cavity. However, due to their disadvantages, extensive research was conducted, leading to the introduction of multiport-VATS, which involved using 3 or 4 ports. This technique quickly evolved into uniportal access (known as uniportal video-assisted thoracic surgery or UNI-VATS), which revolutionized the field. In 2010, the first uniportal lobectomy was performed by Dr. Diego Gonzalez-Rivas, a Spanish thoracic surgeon [1]. In our hospital, UNI-VATS is performed with great expertise by highly qualified surgeons using specialized equipment.
Martin-Ucar and Socci [3] highlighted the various benefits of Uni-VATS, such as reduced post-operative pain, faster recovery, improved visibility of the thoracic cavity, wider angle of vision, absence of rotational effect, and enhanced ergonomics for the operating surgeon. In this technique, a single 2 cm incision is made to create a solitary pleural cavity. This is accomplished by repairing any septal rupture and removing debris from both the visceral and parietal cortex, as well as eliminating inflammatory fluids. Furthermore, there may be a reduced incidence of neuralgia and paresthesia associated with U-VATS, which can be attributed to decreased rib stress angles and minimized nerve compression resulting from the use of fewer instruments. In our experience with U-VATS in children with pleural empyema, we observed these advantages and also discovered additional benefits unique to our single-center setting. Initially, we encountered the challenge of exposing the surgical field as all cases involved severe pleural adhesions that needed to be addressed at the beginning of the procedure.
In larger studies examining the Uni-VATS procedure, only a small subset of patients with early-stage empyema received treatment through single-port access, and no complications or mortality were reported. Our study delves into the technical aspects of Uni-VATS decortication, demonstrating its safety (no postoperative mortality, reduced morbidity) and its effectiveness in terms of disease control (lower recurrence rate) compared to the standard thoracotomy approach. Furthermore, our thoracic surgeons have successfully performed Uni-VATS by utilizing a single incision outside the thorax to treat bilateral empyema thoracic. This procedure has shown significant improvements both radiologically and clinically in all treated patients. Moreover, this technique should require long-term follow-up spanning several years. Furthermore, the non-availability of bronchial blockers and paediatric-sized double-lumen tubes presents a challenge in performing the UNI-VATS technique. Nevertheless, our highly specialized and trained surgeons are demonstrating excellent expertise in performing the procedure without any adverse outcomes. Although the Uni-VATS technique is not widely practiced or recommended in our country due to a lack of training programs, our surgeons are determined to initiate a training program at our hospital. This will enable our future surgeons to gain expertise in this technique.
Based on our observations and the existing published cases, U-VATS emerges as a practical and safe surgical approach for treating lung disorders, particularly empyema decortication. Despite the scarcity of papers on the topic, Uni-VATS has been successfully employed in cardiothoracic pathologies without any significant associated morbidity or mortality. It offers potential additional advantages over traditional VATS, such as a more favorable postoperative experience in terms of pain. These factors make UNI-VATS the optimal procedure of choice for the paediatric population due to its safety, effectiveness, and minimal discomfort.