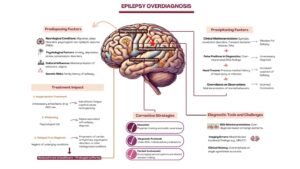
Epilepsy misdiagnosis poses significant challenges, with rates of incorrect diagnoses reaching up to 30% in specialized epilepsy centers. Overreliance on abnormal EEG readings, insufficient standardization of EEG training, and systemic issues in healthcare contribute to the problem. Misdiagnoses often involve alternative conditions, such as psychogenic non-epileptic seizures (PNES), syncope, psychiatric conditions, and sleep disorders. The impact on patients is profound, leading to unnecessary treatment, social stigma, and significant psychological and physical burdens. Healthcare systems face financial strain due to overutilization of resources. Solutions include improved training in EEG interpretation, patient referral to specialized epilepsy centers, EEG machine optimization, and integration of artificial intelligence to enhance accuracy. Biomarkers for epilepsy diagnosis also hold promise. Implementing standardized guidelines, questioning initial diagnoses, and emphasizing clinical correlation over sole reliance on EEG are critical steps toward mitigating epilepsy overdiagnosis and improving patient outcomes.
Epilepsy misdiagnosis is a common problem, with serious, life-altering consequences for patients [1]. Studies indicate that around 23% of epilepsy diagnoses in adult populations may be incorrect [1], while up to 30% of patients diagnosed with refractory epilepsy at specialized centers are misdiagnosed with epilepsy [2]. One primary cause is the tendency to over-read EEG tracings as abnormal; in fact, many erroneous diagnoses rely primarily on an ‘abnormal’ EEG result. Contributing factors to this over-interpretation include insufficient standardization in EEG training and a mistaken assumption that all neurologists are proficient in EEG analysis [3]. Without such interventions, an initial abnormal EEG reading can be nearly impossible to overturn, especially since repeat EEGs may not reliably “cancel” the misdiagnosis, unlike more definitive imaging methods like CT or MRI [4].
Overdiagnosis of epilepsy is more common than underdiagnosis, especially in pediatric populations [5]. Research shows that misdiagnosis is higher in peripheral hospitals and non-specialized settings, where up to 30% of patients, especially children referred for intractable epilepsy, are found to have alternative diagnoses such as syncopal episodes, psychogenic non-epileptic events (NEPEs), or other imitators like neurocardiogenic syncope or benign paroxysmal vertigo [6].
In a retrospective review, 184 patients referred to an epilepsy clinic with a prior diagnosis of epilepsy and undergoing antiepileptic treatment were assessed. The study revealed a misdiagnosis rate of 26.1%, with the most common alternative diagnoses being psychogenic non-epileptic seizures (PNES) and syncope. Notably, over half of these misdiagnosed patients were already receiving antiepileptic medication [7]. In another study that excluded patients with suspected PNES, researchers examined 74 patients referred to an epilepsy clinic, many of whom were initially considered to have refractory epilepsy. The findings indicated that 41.9% of these patients actually had alternative diagnoses, most commonly syncope or other cardiovascular conditions. This highlights the potential for misdiagnosis even among patients presumed to have complex, treatment-resistant epilepsy [8]. This issue is further complicated by the diversity of seizure symptoms, ranging from sensory changes to psychogenic factors, making diagnosis challenging without advanced tools like video EEG (v-EEG), the gold standard for differentiating epilepsy from NEPEs [9, 10].
The heterogeneity in misdiagnosis rates across studies reflects differences in healthcare settings, diagnostic approaches, and the experience level of referring clinicians. Gender and age groups are also factors, with higher misdiagnosis rates observed in children, who often rely on parental or caregiver observations rather than direct assessments, which are difficult to achieve in many pediatric and non-specialized facilities [11]. The diagnostic information obtained from a single interictal EEG is low; it is frequently normal in children with epilepsy and 2-5% of children without epilepsy present with epileptiform EEG discharges, especially in the centrotemporal regions. Furthermore, several benign variant patterns not related to epilepsy are often misinterpreted as epileptiform [11]. Another study, which excluded patients with suspected psychogenic non-epileptic seizures (PNES), found that among 74 patients referred to an epilepsy clinic—half of whom were believed to have refractory epilepsy—41.9% were instead found to have alternative diagnoses, most commonly syncopal or cardiovascular causes for their symptoms [8].
Numerous medical and psychiatric conditions can often be misdiagnosed as epilepsy [1]. Cardiovascular syncope is sometimes mistaken for seizures in all age groups [12]. Drug-induced tics are often misdiagnosed as convulsive automatism. These tics in the elderly are usually secondary to common neurologic drugs used in this population including neuroleptics, levodopa, and sympathomimetic agents. Moreover, intermittent episodes of confusion may be misinterpreted as focal impaired awareness seizures (FIAS), when they are episodes of transient ischemic attacks, prodromal stage of dementia, or simply age-related cognitive decline. Lastly, sometimes unresponsiveness or even loss of balance and falls secondary to orthostatic hypotension, vasovagal syncope, or more importantly convulsive syncope, may all be wrongly diagnosed as FIAS [13].
On the other hand, another common non-epileptic condition that may be misdiagnosed as seizures is Sandifer Syndrome in children [14]. This condition requires a high index of suspicion. Effectively, the generalized body stiffening experienced by patients suffering from Sandifer syndrome often leads both parents and physicians to confuse these intermittent paroxysmal spells of dystonia for epileptic events [15]. Moreover, this complication of gastroesophageal reflux disease is often missing from the differential diagnosis of many neurologists and thus may be more common than officially reported. Three important features to help differentiate Sandifer syndrome from epilepsy are first the lack of paroxysmal events during sleep, second the lack of impaired awareness and the individual remaining conscious throughout the spell, and third the normal neurological exam [16].
Note that various psychological and psychiatric events like hallucinations, paroxysmal non-epileptic seizures, tantrums, and rage reactions, in addition to sleep disorders, are commonly classified as epileptic events [12].
Epilepsy overdiagnosis is a significant issue in healthcare and leads to unnecessary treatments and high psychological stress for some patients [1]. Factors leading to overdiagnosis include: human mistakes, difficulties in interpreting and misreading EEG results, misunderstandings about epilepsy pathophysiology, similarities with other conditions, differences in diagnostic methods across different centers, and over-referral [17, 18, 19, 20, 21, 22, 23, 24, 25].
Overreliance on EEG without clinical correlation has been cited as one of the main causes of epilepsy overdiagnosis [17]. Kwan et al. (2020) highlight a critical issue: many general neurologists and neurology residents are not sufficiently trained in EEG analysis during residency years, which causes a major part of diagnostic inaccuracy. The authors state that a broader approach that focuses on the correlation between EEG data and more extensive clinical examinations is necessary in order to minimize some mistakes Figure 1 [17].
The interpretation of EEGs is generally considered to be a complex and subjective process even when patterns that are deemed to be benign are frequently mistaken for epileptiform discharges. In a systematic review by Oto et al. [18], authors paid much attention to the fact that normal EEG variants including wicket spikes and nonspecific background fluctuations are often mistaken for pathological changes. The review underlines the role of context analysis as the diagnostic role of EEGs without proper attention to the clinical circumstances entails large diagnostic errors [18]. Fisher et al. [19] build on false-positive EEG overreading, where the interpreters became unaware and biased by a patient’s previous seizure history thereby providing misleading results.
Lack of proper knowledge regarding the first seizures and their management contributes a lot to the overdiagnosis of epilepsy. Berg et al. [20] discussed the widespread belief that early treatment after an initial seizure can lead to better outcomes hence contributing to early EEG referral. Due to this, many healthcare practitioners have been recommending patients for EEG tests even when clinical evidence does not strongly suggest epilepsy. This paper found out that many of these referrals are unnecessary and actually, many of the patients do not have epilepsy [20]. O’Toole et al. [24] indicated that 66% of EEG requests were inappropriate, especially in patients presenting with symptoms such as syncope that are atypical. At least 30% of EEG requests have been reported by guidelines as not meeting the clinical criteria [21]. According to ILAE (2021), many EEGs are requested when the justification is not readily available lowering the value of these tests [25].
Diagnostic practices in the peripheral hospitals also perpetrate overdiagnosis of epilepsy as compared to the central hospitals. According to [22], it was found that peripheral hospitals resort to EEG overreading more often than tertiary referral centers, which employ specialized epilepsy professionals. The overdiagnosis of such conditions is even more common when EEG interpretation is done in peripheral centers, where access to trained neurophysiologists is rare. The study calls for a more rational distribution of personnel, other resources, and focused training programs in peripheral hospitals to enhance diagnostic accuracy and reduce overreliance on EEG results.
Seizure-like clinical scenarios make the diagnosis of epilepsy more challenging. [23] highlight the challenges that doctors experience while trying to differentiate epilepsy from other mimics such as psychogenic non-epileptic spells. Such overlap of semiology usually confuses and frequently patients are diagnosed with both instead of one. Thus the study emphasizes the need to extend a diagnostic assessment including routine EEG to detailed clinical assessment combined with long-term video EEG recording, providing crucial proof to differentiate between epileptic and non-epileptic events.
Epilepsy is more commonly overdiagnosed than underdiagnosed, with serious consequences for both the patient and the physician [26]. Some physicians describe it as an “Erroneous Diagnosis of Epilepsy”, mostly due to EEG over-analysis and other factors described previously [26, 27]. However, the problem is not just the “error” in diagnosis but most importantly the impact this diagnosis leaves on these patients. Once diagnosed with epilepsy, the patient is followed by a lifelong “label” regularly repeated in all their medical records, a label now becoming a significant part of their life: this includes the physical, psychological, emotional as well as financial aspects of their life [26, 27]. This can negatively affect their employment status, insurance difficulties, and the stigma associated with working and public spaces like social marginalization, lifestyle limitations, and driving restrictions [18, 26, 27]. Additionally, the patient can be exposed to unnecessary side effects and potential teratogenic effects of AEDs [18]. The impact of epilepsy misdiagnosis on individual patients and broader healthcare systems is summarized in Table 1.
| Impact Area | Consequences |
|---|---|
| Patient Impact | Missing the Correct Diagnosis: Delays in identifying actual conditions (e.g., cardiovascular issues like arrhythmias), which can be life-threatening. |
| Prolonged Misdiagnosis: Patients can live with the misdiagnosis for 7-10 years before receiving the correct diagnosis. | |
| Overtreatment: Unnecessary prescription of AEDs, exposing patients to risks such as liver toxicity and cognitive impairment. | |
| Psychiatric Morbidity: Misdiagnosed patients may experience untreated psychiatric issues, worsening their mental health. | |
| Psychological Effects: The stigma of epilepsy leads to anxiety, depression, and social isolation. Lifestyle restrictions (e.g., driving) worsen this effect. | |
| Iatrogenic Harm: Misdiagnosed patients may receive unnecessary high doses of intravenous medication or ICU care, increasing the risk of harm. | |
| Side Effects of AEDs: Unnecessary use of AEDs can lead to side effects like fatigue, dizziness, and cognitive decline without benefit. | |
| Healthcare Impact | Financial Burden: Misdiagnosis leads to unnecessary costs for diagnostic tests, medications, and hospitalizations. |
| Overutilization of Resources: Non-epileptic patients receiving epilepsy treatment strain healthcare resources. | |
| Costs of Correcting Diagnosis: Reversing a misdiagnosis requires expensive diagnostic tests like video EEG monitoring and inpatient care. |
Understanding the problem and consequences of epilepsy overdiagnosis is key to avoiding it [18]. The first step to solving this problem is to question the real need to prescribe this EEG and how much it will contribute to the diagnosis, management, and prognosis of the patient. Then clinicians should take into consideration that the diagnosis might be wrong and that it should be routinely questioned and reviewed. Introducing a category labeled “possible epilepsy” or “unclassified paroxysmal event” decreases the number of patients incorrectly labeled as epileptic [3, 18].
The interpretation of the EEG should be considered along with the clinical and psychological history of the patient and the population at high risk of cardiogenic syncope and paroxysmal non-epileptic seizures should be recognized. But, to avoid the looking too hard syndrome or history bias, it is advised that the EEG is read by an EEGer who doesn’t know the patient’s history [3, 28].
Since experts tend to adopt diagnostic uncertainty more than non-experts, consultation of an epileptologist and EEG specialist is to be considered and a confirmatory EEG reading by an EEGer should be provided [3]. It has been recognized that less experience lowers the threshold for clinicians to find abnormalities while reading EEGs, hence, residency programs should introduce a quality EEG training program. App-based learning models have been developed to help residents. These models give immediate feedback to them if they classify correctly the EEG changes [3].
Although the field is not yet well developed, and the use of inflammatory biomarkers is not yet well introduced while diagnosing and managing epilepsy, they carry promising results in epilepsy diagnosis and quantification of the response to treatment. S100 calcium-binding protein B (S100B), neuronal specific enolase (NSE), glial fibrillary acidic protein (GFAP), neurofilament light protein (NfL), microtubule-associated protein tau (Tau), ubiquitin C-terminal hydrolase 1 (UCHL-1), and metalloproteinase 9 (MMP-9) are among the known and studied candidates. These markers originate in the brain and are present in neural tissues [29].
Many algorithms have been developed to enhance the accuracy of EEG readings, each with unique features contributing to better identification of epileptiform discharges and epilepsy risk. The Bergen Epileptiform Morphology Score (BEMS) is a validated, reproducible scale ranging from 0 to 86, with higher scores indicating more typical epileptiform morphology. Its calculation is based on spike slope, amplitude, background similarity, slow after-wave area, and patient age, as morphology depends on age. This scale is predictive of future epilepsy [30, 31]. An alternative, the Halford semiquantitative scale, offers similar diagnostic performance but with lower reproducibility [31].
Artificial intelligence (AI) models have also made significant strides in EEG classification. SpikeNet, a deep neural network, has demonstrated expert-level accuracy [32]. Many other artificial intelligence models like Wave_clus, an automatic spike-sorting algorithm, classify interictal epileptiform discharges (IED) that are visually identified and reduce the workload of the clinical electrophysiologist [33].
Artifacts and noise caused by other muscle activity can result in normal benign variants that can be easily mistaken for epileptiform discharges. Various methods have been employed to denoise the EEG, among which are the regression method, blind source separation, canonical correlation analysis, wavelet transform, and empirical method decomposition. All these methods consist of detecting the signal and noise during EEG recording and deducting the noise to obtain an optimal reading without artifacts Algorithm 2, [34].

The EEG and MRI are part of the seizure workup [35, 36]. To avoid EEG overreading, clinicians should avoid overprescribing EEGs [3]. Before ordering an EEG for a patient, clinicians should ask themselves if there is a real need for the recording and if it will contribute to the diagnosis, management, or prognosis of the patient [3, 37]. EEG prescriptions should follow clear and specific guidelines [38]. If there is a real need for the EEG, it should first be read by the neurologist who ordered it and separately by an artificial intelligence model, standardizing all factors [32, 39, 40, 41]. If no epileptiform discharges are found, a correlation with neuroimaging results and the clinical picture is needed to decide the diagnostic and therapeutic approach [36]. A more prolonged recording, including all potential precipitating factors, may be considered to increase the likelihood of detecting epileptiform discharges [18, 26, 42].
If the clinician is uncertain about the presence of epileptiform discharges, the case should be labeled as either “possible epilepsy” or an “unclassified paroxysmal event” [29]. In both cases, a neurophysiology expert should review the EEG both before and after considering the patient’s history [3]. If the expert confirms the presence of epileptiform discharges, the diagnosis of epilepsy is established [36]. However, if the expert remains uncertain about the presence of epileptiform discharges or the EEG changes are considered benign, the approach should rely on clinical suspicion, as epilepsy is primarily a clinical diagnosis, and a normal EEG does not rule it out [26, 35]. When clinical suspicion is high and the patient’s presentation is typical, the diagnosis of epilepsy should be considered [26]. If the clinical picture and neuroimaging are inconclusive, consider the possible benefit of inflammatory biomarkers [29]. Or repeated/prolonged EEG recordings [18, 26]. If the diagnosis remains unclear, the patient should be followed clinically without initiating treatment [36].
Scheepers B, Clough P, Pickles C. The misdiagnosis of epilepsy: findings of a population study. Seizure. 1998 Oct;7(5):403-6.
Benbadis SR, O’Neill E, Tatum WO, Heriaud L. Outcome of Prolonged Video-EEG Monitoring at a Typical Referral Epilepsy Center. Epilepsia. 2004 Sep;45(9):1150-3.
Benbadis SR. The tragedy of over-read EEGs and wrong diagnoses of epilepsy. Expert Rev Neurother. 2010 Mar;10(3):343-6.
LaFrance WC, Benbadis SR. Avoiding the costs of unrecognized psychological nonepileptic seizures. Neurology. 2006 Jun 13;66(11):1620-1.
Benbadis SR. Psychogenic seizures. e Medicine Journal. 2001. Available at: http://www.emedicine.com/neuro/topic403.htm
Uldall P. The misdiagnosis of epilepsy in children admitted to a tertiary epilepsy center with paroxysmal events. Archives of Disease in Childhood. 2006 Mar 1;91(3):219-21.
Smith D. The misdiagnosis of epilepsy and the management of refractory epilepsy in a specialist clinic. QJM. 1999 Jan 1;92(1):15-23.
Zaidi A, Clough P, Cooper P, Scheepers B, Fitzpatrick AP. Misdiagnosis of epilepsy: many seizure-like attacks have a cardiovascular cause. Journal of the American College of Cardiology. 2000 Jul;36(1):181-4.
Benbadis SR, Allen Hauser W. An estimate of the prevalence of psychogenic nonepileptic seizures. Seizure. 2000 Jun;9(4):280-1.
Seneviratne U, Reutens D, D’Souza W. Stereotypy of psychogenic nonepileptic seizures: Insights from video-EEG monitoring. Epilepsia. 2010 Jul;51(7):1159-68.
Foldvary N. Normal electroencephalogram and benign variants. In: Levin K, Lüders HO, eds. Comprehensive Clinical Neurophysiology. Philadelphia: Saunders, 2000.
Epilepsy Imitators. (n.d.). https://www.epilepsydiagnosis.org/epilepsyimitators.html
Davis Jr V, Desai D, Udernani B. The Ultimate Shake Down: Epilepsy vs. Syncope. https://www.preprints.org/manuscript/202312.2248/v1
Mindlina I. Diagnosis and management of Sandifer syndrome in children with intractable neurological symptoms. European Journal of Pediatrics. 2020 Feb;179(2):243-50.
Moore DM, Rizzolo D. Sandifer syndrome. JAAPA. 2018 Apr;31(4):18-22.
Patil S. Sandifer syndrome. StatPearls. (2023, June 20).
Kwan P, Schachter SC, Brodie MJ. Drug-Resistant Epilepsy. The New England Journal of Medicine. 2011 Sep 8;365(10):919-26.
Oto M (Meritxell). The misdiagnosis of epilepsy: Appraising risks and managing uncertainty. Seizure. 2017 Jan;44:143-6.
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. ILAE Official Report: A practical clinical definition of epilepsy. Epilepsia. 2014 Apr;55(4):475-82.
Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, Van Emde Boas W, et al. Revised terminology and concepts for organization of seizures and epilepsies: Report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia. 2010 Apr;51(4):676-85.
National Center for Biotechnology Information (NCBI). Guidelines for the use of EEG in epilepsy diagnosis. 2020. Available at: https://www.ncbi.nlm.nih.gov
Schiltz NK, Koroukian SM, Singer ME, Love TE, Kaiboriboon K. Disparities in access to specialized epilepsy care. Epilepsy research. 2013 Nov 1;107(1-2):172-80.
Bodde NM, Brooks JL, Baker GA, Boon PA, Hendriksen JG, Aldenkamp AP. Psychogenic non-epileptic seizures—diagnostic issues: a critical review. Clinical neurology and neurosurgery. 2009 Jan 1;111(1):1-9.
O’Toole J, Dupuis N, Taylor R. The value of EEG in the assessment of first seizures: A prospective evaluation. Epilepsia. 2009;50(2):383-391.
International League Against Epilepsy (ILAE). Guidance on the appropriate use of EEG. Epilepsia. 2021;62(1):85-92.
Amin U, Benbadis SR. The Role of EEG in the Erroneous Diagnosis of Epilepsy. Journal of Clinical Neurophysiology. 2019 Jul;36(4):294-7.
Benbadis SR. Errors in EEGs and the misdiagnosis of epilepsy: Importance, causes, consequences, and proposed remedies. Epilepsy Behav. 2007 Nov;11(3):257-62.
Devinsky O, Gazzola D, LaFrance WC. Differentiating between nonepileptic and epileptic seizures. Nature Reviews Neurology. 2011 Apr;7(4):210-20.
Banote RK, Akel S, Zelano J. Blood biomarkers in epilepsy. Acta Neurologica Scandinavica. 2022 Oct;146(4):362-8.
Aanestad E, Gilhus NE, Olberg HK, Kural MA, Beniczky S, Brogger J. Spike count and morphology in the classification of epileptiform discharges. Frontiers in Neurology. 2023 May 23;14:1165592.
Aanestad E, Gilhus NE, Brogger J. A new score for sharp discharges in the EEG predicts epilepsy. Journal of Clinical Neurophysiology. 2023 Jan;40(1):9-16.
Jing J, Sun H, Kim JA, Herlopian A, Karakis I, Ng M, Halford JJ, Maus D, Chan F, Dolatshahi M, Muniz C. Development of expert-level automated detection of epileptiform discharges during electroencephalogram interpretation. JAMA Neurology. 2020 Jan 1;77(1):103-8.
Sharma NK, Pedreira C, Centeno M, Chaudhary UJ, Wehner T, França LG, Yadee T, Murta T, Leite M, Vos SB, Ourselin S. A novel scheme for the validation of an automated classification method for epileptic spikes by comparison with multiple observers. Clinical Neurophysiology. 2017 Jul 1;128(7):1246-54.
Saeidi M, Karwowski W, Farahani FV, Fiok K, Taiar R, Hancock PA, Al-Juaid A. Neural decoding of EEG signals with machine learning: a systematic review. Brain Sciences. 2021 Nov 18;11(11):1525.
King MA, Newton MR, Jackson GD, Fitt GJ, Mitchell LA, Silvapulle MJ, Berkovic SF. Epileptology of the first-seizure presentation: a clinical, electroencephalographic, and magnetic resonance imaging study of 300 consecutive patients. The Lancet. 1998 Sep 26;352(9133):1007-11.
Rizvi S, Ladino LD, Hernandez-Ronquillo L, Téllez-Zenteno JF. Epidemiology of early stages of epilepsy: Risk of seizure recurrence after a first seizure. Seizure. 2017 Jul;49:46-53.
Hasan TF, Tatum WO. When should we obtain a routine EEG while managing people with epilepsy?. Epilepsy & Behavior Reports. 2021 Jan 1;16:100454.
Birbeck GL, Chomba E, Ataadzhanov M, Haworth A, Mbewe E, Mpabalwani EM. Neurological & psychiatric society of Zambia’s evidence-based guidelines for EEG utilization at the university teaching hospital. Medical Journal of Zambia. 2011;38(3):9-15.
Tveit J, Aurlien H, Plis S, Calhoun VD, Tatum WO, Schomer DL, Arntsen V, Cox F, Fahoum F, Gallentine WB, Gardella E. Automated interpretation of clinical electroencephalograms using artificial intelligence. JAMA Neurology. 2023 Aug 1;80(8):805-12.
Van Leeuwen KG, Sun H, Tabaeizadeh M, Struck AF, Van Putten MJAM, Westover MB. Detecting abnormal electroencephalograms using deep convolutional networks. Clinical Neurophysiology. 2019 Jan;130(1):77-84.
Barnett AJ, Guo Z, Jing J, Ge W, Kaplan PW, Kong WY, Karakis I, Herlopian A, Jayagopal LA, Taraschenko O, Selioutski O. Improving clinician performance in classifying EEG patterns on the ictal–interictal injury continuum using interpretable machine learning. NEJM AI. 2024 May 23;1(6):AIoa2300331.
Chen H, Koubeissi MZ. Electroencephalography in epilepsy evaluation. CONTINUUM Lifelong Learning in Neurology. 2019 Apr;25(2):431-53.